Here are some ugly truths: Women and men experience pain differently. Doctors are less likely to treat women’s pain. Health issues that disproportionately affect women are not studied as much as those affecting men. It can take women multiple visits and sometimes years to diagnose their medical issues and chronic illnesses. And when painful conditions like Endometriosis and Fibromyalgia don’t have a simple test for diagnosing, those visits and months and years can prove both emotionally and physically draining when you’re already in pain and still having to fight for a diagnosis.
Pain is Pain…
No matter what the cause, pain is pain. From Fibromyalgia and chronic neck and back pain to years of suffering from Endometriosis, I know pain. I know what it’s like to go to doctor after doctor, having test after test, to find out what is wrong with you. Because you KNOW there’s something wrong, even if it doesn’t show up on their tests.
“The only thing that kept me strong enough to make it to my seventeenth doctor was hearing the stories of other women who had persevered.”
From “What to Know about Chronic Illness, from Someone Who Visited 17 Doctors Before a Diagnosis”
And when you keep coming up empty-handed, your stress and anxiety levels can increase until one day you are a blubbering idiot at the physical therapist’s office or the orthopedic specialist’s office or at your primary care doctor. True story. I have cried at all three, pleading with someone to recognize my pain and help me.
This article highlights the 20 Most Painful Conditions you can have. I have had or currently live with 8 of those conditions. Fibromyalgia and endometriosis are just two of them that I will share here.
Fibromyalgia
“Fibromyalgia is a common neurologic health problem that causes widespread pain and tenderness (sensitivity to touch). The pain and tenderness tend to come and go, and move about the body. Most often, people with this chronic (long-term) illness are fatigued (very tired) and have sleep problems.”
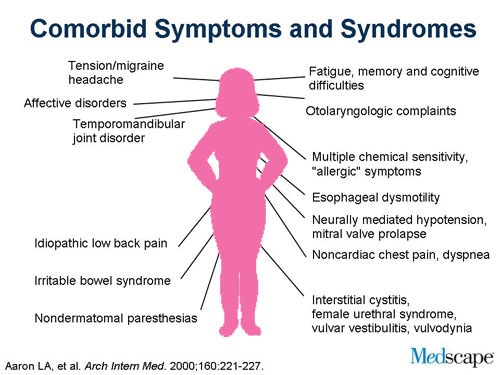
Fibromyalgia has a high occurrence of misdiagnosis, symptoms overlap with many other conditions, and it has a high rate of co-morbidity with other conditions. Getting to a diagnosis may be a chore in and of itself, first ruling out other things.
For me, luckily, it only took four months to get to my diagnosis. But it was in part thanks to a great primary care doctor who believed me, as well as research my mom and I had done ourselves. (You can never be too educated!) When I started showing the most severe symptoms, my doctor ran blood work and I had some strange blood results on my ANA (anti-nuclear anti-body), which led to a referral to a rheumatologist. And then it took months to get in to see one as a new patient, but persistence and patience got me through.
Diagnosis for me came from him reviewing my blood work, interview/examination, and examining the above tender points. They used to say if you had widespread pain and tenderness in 11 of these 18 areas, it was fibromyalgia. In 2010, the College of Rheumatology moved past the “tenderness” scale and came up with this criteria for diagnosing Fibromylagia:
- You have a widespread pain index (WPI) score of seven or higher and a symptom severity scale (SS) score of five or higher. Or you have a WPI score of three to six and a SS score of nine or higher.
- You’ve experienced symptoms at a similar level for at least 3 months.
- You don’t have another disorder that could explain your symptoms.
The last bullet means they have to run tests to rule out other things. This can be blood tests, ultrasounds, X-Rays, CT-Scans. In other words, expensive tests. These days there is new research showing widespread inflammation in the brain in those with fibromyalgia. While this won’t necessarily change the course for diagnosing, it does back-up the fact that these patients do have something wrong with them.
Endometriosis
In the 27 years since I was first diagnosed with endometriosis, there is still is no simple test to diagnose this condition; it is diagnosed through surgery. As such, doctors will typically will rule various things out and run a variety of tests before proceeding with a laparoscopic procedure. What helped me help my doctor? Keeping a journal of my pain and symptoms in relation to my monthly cycles. The diagnoses still took several months and tests – ultrasounds, upper GI, lower GI, ER visits to rule out things such as appendicitis and gallstones.
My pain was so severe at times I nearly passed out. The right side of my body would go numb, from endometrial tissue on back muscles and likely my sciatic nerve. Read more on endometriosis.
The treatment for me was multi-faceted over many years. First was the laparoscopy for the initial diagnosis and removal. Then years of hormone therapy to suppress it. Thankfully, I was able to have two children, but after my second was born there was more endometrial tissue to be removed. I endured numerous procedures and treatments for 20 years before finally having a hysterectomy to end the pain.
Your Journey
Here are some other blogs I have written that might help you along your journey to diagnosing what ails you:
- Becoming Your Own Health Advocate
- Fibromyalgia Symptom Round-up
- When Everything Hurts
- Lessons Learned in Diagnosing Chronic Pain
Above all else, I highly recommend keeping a medical journal, to track symptoms, level of pain, and reactions to medications. The process of getting diagnosed can lead to excess anxiety and stress as well, which oftentimes exacerbates the pain and adds more symptoms and issues into the mix. Write it all down!

Make sure you are describing your symptoms and your pain levels accordingly. Is the pain dull? Sharp? Hot/burning? Cold/freezing? Stinging? Does it come and go or stay steady? Does it get better/worse or stay the same?
And once you get a diagnosis, that is just the beginning. Then you have to find that combination of therapies (drug or otherwise) that work for you.
My Journey
Relatively speaking, my journey to diagnosing fibromyalgia and endometriosis were short. I attribute both of these to the fact that I educated myself. And these were both back before the days of the internet, so going to libraries and book stores to find medical books was all I had.
Treatment, on the other hand, has been a process over the years. In addition, I have had other long, drawn out episodes of multiple doctors and tests in diagnosing both a herniated disc in my neck (15 months from the first pain to the surgery to repair) and my frozen shoulder (22 months from the first pain to pain relief and now on-going physical therapy). So don’t think I am any stranger to the pain and agony of the medical diagnoses process.
“Keep the faith, don’t lose your perseverance, and always trust your gut instinct.” ~ Paula Abdul
If you know in your gut something is wrong, don’t give up in finding the answers. Perseverance will see you to the end!
Have you had similar experiences with getting something diagnosed? Do you have other strategies you recommend for getting proper medical care and attention? Please leave me a comment below. I would love to hear from you!

P.S. I would also ❤ for you to follow my blog and follow me on social media. You can find all the ways to follow me here.




One suggestion is to not suggest your diagnosis to the doctor. Give all the symptoms of said diagnosis. Let it be them be the one that names it.
I’ve also said ”I’ve been told I have xyz “ but you are the doctor!
Playing “dumb” sometimes works.
LikeLiked by 1 person
Yes of course, they are the professionals!! Thank you!
LikeLiked by 1 person
Finding a physician who believes Fibromyalgia is actually a illness is important…otherwise they can become dismissive…
Things have improved in the last decade with more research finding physiological evidence to our symptoms.
Jennifer
LikeLiked by 1 person